The Rise of Ozempic
Ozempic, or semaglutide, was introduced to the market with high expectations. Developed by Novo Nordisk, it belongs to a class of drugs known as GLP-1 receptor agonists. Initially approved for the treatment of Type 2 diabetes, Ozempic promised to manage blood sugar levels effectively and aid in weight loss. Its effectiveness and relative safety earned it widespread acclaim.
What Is Ozempic?
Ozempic works by mimicking the effects of the GLP-1 hormone, which plays a role in regulating blood sugar levels and appetite. By activating GLP-1 receptors, Ozempic helps increase insulin production, decrease glucagon release, and slow down gastric emptying, which can lead to reduced appetite and weight loss.
The Initial Euphoria
Upon its release, Ozempic was quickly embraced by the medical community and patients alike. Its dual action of controlling blood glucose and promoting weight loss made it a promising option for many individuals struggling with Type 2 diabetes. Clinical trials showed significant improvements in HbA1c levels and body weight, leading to its widespread adoption.
The Controversy Begins
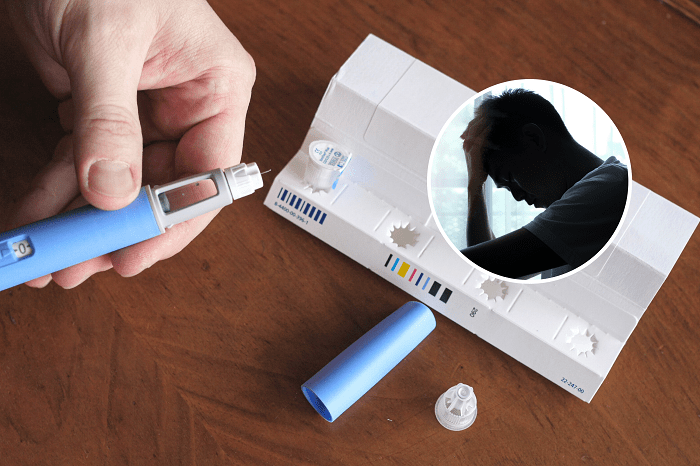
Despite its initial success, recent developments have cast a shadow over Ozempic’s reputation. Reports of adverse effects, discrepancies in research data, and regulatory concerns have raised questions about the drug’s safety and efficacy.
Allegations of Misleading Data
One of the central issues revolves around allegations that the data supporting Ozempic’s efficacy was misleading. Some critics argue that the clinical trials did not fully disclose the range of potential side effects or the drug’s long-term impact. This lack of transparency has fueled skepticism and calls for a reevaluation of the drug’s benefits versus its risks.
Adverse Effects and Side Effects
As more patients began using Ozempic, reports of side effects emerged. While some side effects were expected, such as gastrointestinal issues, others were more concerning. Reports of severe pancreatitis, thyroid cancer, and kidney problems led to increased scrutiny from health professionals and regulatory agencies.
The Weight Loss Debate
Ozempic’s weight loss benefits were initially seen as a bonus for diabetic patients struggling with obesity. However, some experts argue that promoting the drug as a weight-loss solution may have overshadowed its primary function as a diabetes medication. This shift in focus has led to debates about the drug’s intended use and its long-term implications.
Scientific Examination: What Went Wrong?
To understand what went wrong with Ozempic, we need to examine the scientific and regulatory aspects that contributed to the controversy.
Clinical Trial Design and Reporting
Clinical trials are the cornerstone of medical research, but their design and reporting can significantly impact the perceived efficacy and safety of a drug. For Ozempic, questions have arisen about the trial protocols and the completeness of data reporting.
Methodological Concerns
Some experts have pointed out methodological concerns in Ozempic’s clinical trials. These include issues related to sample sizes, control groups, and statistical analyses. Such concerns can influence the reliability of the reported outcomes and lead to misleading conclusions about the drug’s effectiveness and safety.
Data Transparency
Transparency in clinical research is crucial for building trust and ensuring that all potential risks and benefits are accurately conveyed. Critics argue that certain data regarding Ozempic’s side effects and long-term risks may not have been fully disclosed, raising concerns about the drug’s overall safety profile.
Regulatory Oversight
Regulatory agencies like the FDA play a vital role in evaluating and approving medications. However, regulatory processes are not infallible, and oversight can sometimes fall short. The scrutiny of Ozempic’s approval process has led to questions about whether adequate measures were in place to assess the drug’s safety and efficacy comprehensively.
Approval Process
The approval process for Ozempic involved rigorous evaluations, but some critics argue that the drug was fast-tracked due to its promising initial results. This expedited approval may have led to less thorough examination of potential risks, contributing to the current controversy.
Post-Market Surveillance
Post-market surveillance is essential for monitoring a drug’s performance and safety after it has been approved. Concerns have been raised about whether adequate post-market surveillance was conducted for Ozempic and whether emerging issues were addressed in a timely manner.
The Impact on Patients
The controversy surrounding Ozempic has significant implications for patients who rely on the drug for managing their diabetes and weight. Understanding the impact on patients involves examining both the benefits and the risks associated with the medication.
Patient Experiences
Many patients initially experienced positive outcomes with Ozempic, including improved blood sugar control and weight loss. However, the emergence of adverse effects has led to varying experiences among users. Some patients have reported severe side effects, leading to a reevaluation of the drug’s overall value.
The Need for Alternatives
As questions about Ozempic’s safety and efficacy continue, patients and healthcare providers may seek alternative treatments. The availability of other diabetes medications and weight management options can provide alternatives for those who are concerned about the risks associated with Ozempic.
Future Directions and Recommendations
The Ozempic controversy highlights the need for ongoing research, transparency, and vigilance in the medical field. Addressing the issues requires a multifaceted approach that involves reevaluating the drug’s safety profile and improving regulatory practices.
Reevaluation of Efficacy and Safety
Ongoing research and independent reviews are essential for reassessing Ozempic’s efficacy and safety. This includes conducting new clinical trials, analyzing real-world data, and addressing any gaps in the current understanding of the drug’s effects.
Enhancing Transparency
Transparency in clinical research and regulatory processes is crucial for maintaining trust and ensuring that patients and healthcare providers have accurate information. Efforts to improve data reporting and disclosure can help address concerns and enhance the overall quality of medical research.
Strengthening Regulatory Oversight
Regulatory agencies must continually refine their processes to ensure comprehensive evaluations of new medications. This includes implementing robust post-market surveillance programs and addressing any emerging issues promptly.
Related Post:
Chicago Cubs vs Texas Rangers: Match Player Stats Breakdown
Red Sox vs Pittsburgh Pirates Match Player Stats: A Comprehensive Breakdown
Colorado Rockies vs White Sox Match Player Stats
The controversy surrounding Ozempic underscores the complexities of modern medicine and the importance of rigorous scientific evaluation. While the drug initially offered promising benefits, recent developments have raised critical questions about its safety and efficacy.
As we move forward, it is crucial to address these concerns through continued research, transparency, and enhanced regulatory oversight. By learning from the Ozempic experience, we can work towards ensuring that future medications are both effective and safe for patients.